Summer 2016
The Economic Crisis, Addiction, and Suicide
Rising mortality rates hit rural, white America hard.
More Russians died when the Cold War ended than during it. Male life expectancy fell by seven years in the space of just five years. Female life expectancy fell by three years. People were dying in the primes of their lives – the mortality rate among men aged 35-44 rose by 74%. On the surface, the causes seemed inexplicable: there were no battles, no epidemics, no attacks.
Now something similar is happening in America.
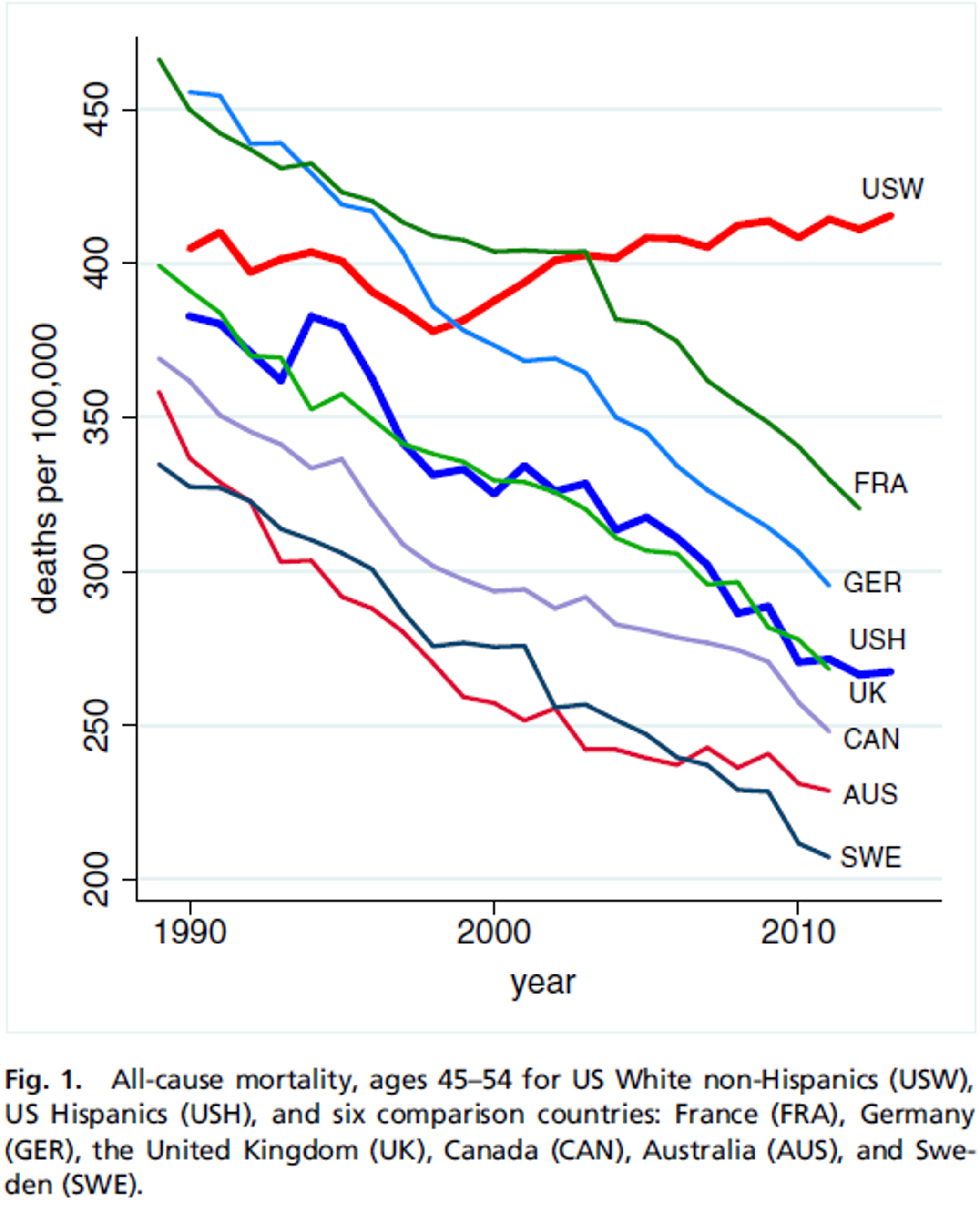
Between the end of the Second World War and the new millennium (with a brief pause in the 60’s because of deaths related to smoking), the U.S. mortality rate fell by an average of about 2% each year for all demographics, as it has in other developed countries. But starting in 1999, the decline in deaths has halted for white Americans. At the end of 2015, Angus Deaton, the most recent Nobel laureate in Economics, and his wife and fellow Princeton economist Anne Case published a paper that demonstrated an increase in mortality and morbidity among white Americans aged 45-54, especially among those with a high school education or less, and especially in rural areas.
Several statisticians have come forward to dispute Case and Deaton’s numbers, saying that the numbers are skewed because the (huge) baby boomer generation was young at the beginning of the time period being studied and older by the end, with the higher mortality rate that implies. This has been balanced by subsequent studies that show higher mortality rates extending throughout the 19-65 age group in the white demographic. But even if the critics are correct, their corrections only change the death rates from an actual increase in mortality to a leveling off, a halt in the historic decline of deaths. That makes for a less impressive headline, but the implications are still staggering. It means that something is counteracting all of the advances in medicine of the past six decades, all of the extension of services including the increases in coverage brought about by the Affordable Care Act, and all improvements in health behaviors like smoking and eating.
Deadly Pessimism
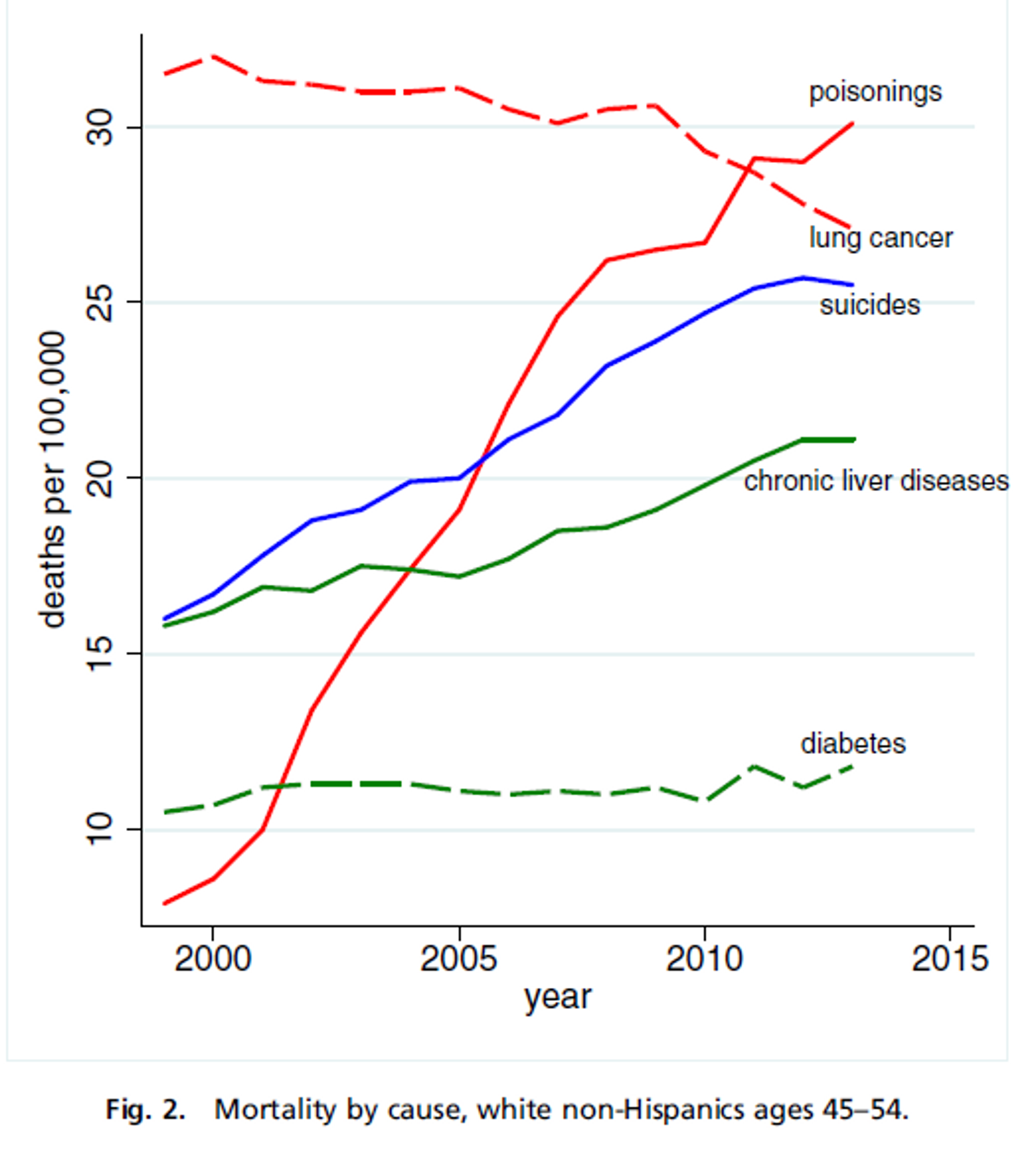
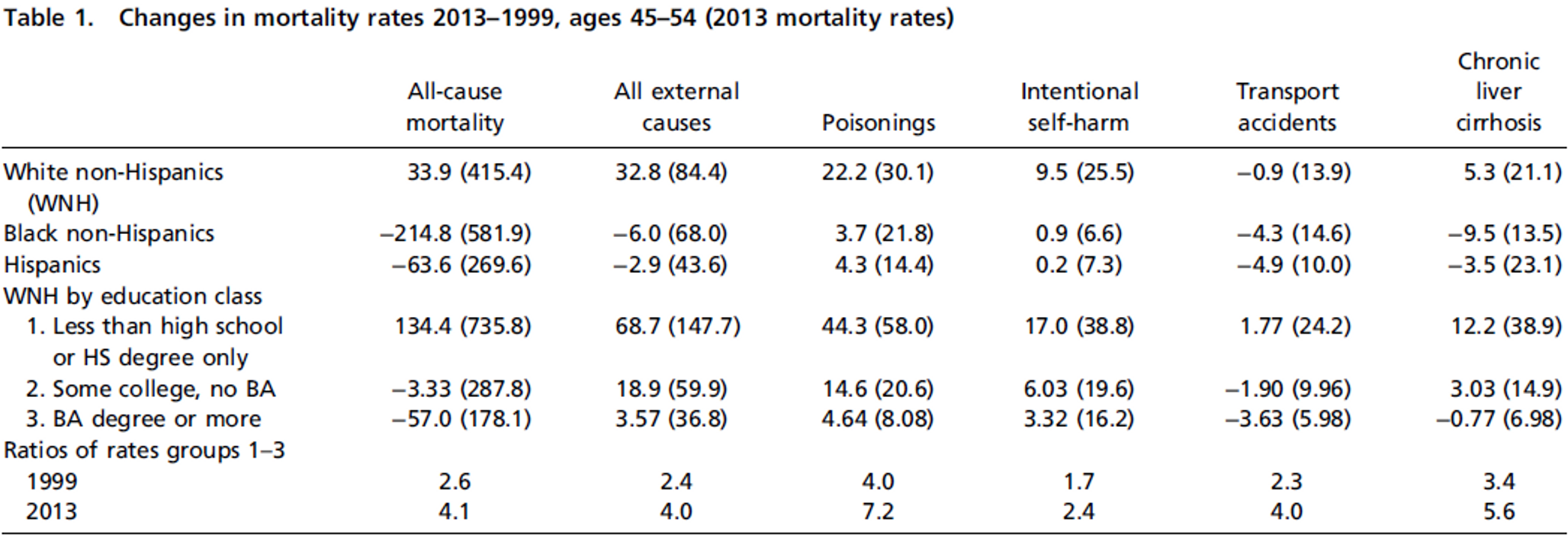
Case and Deaton point to three main causes of this increase in deaths: poisonings from drug overdoses, deaths from liver diseases (likely related to alcoholism), and suicides. The Commonwealth Fund found that the lack of progress in several leading causes of death such as heart disease was also a major factor. This is highly reminiscent of Russia in the 1990s, when rising deaths from heart disease were attributed to increased economic stress because no other risk factors appear to have changed.
Financial hardship is strongly correlated with rises in suicide rates and substance abuse, and the economic collapse in America’s heartland can’t be overlooked as a factor in the rise of American deaths.

The town of Trenton, Georgia has a population of just over 2,000, and when the Shaw Industries Group closed its yarn factory there in 2009, it lost almost 500 jobs. This is the story of hundreds of rural communities across the country over the past two decades, as demand shifted and trade liberalization and advanced technologies brought massive restructuring of supply chains. Many of these communities never recovered, and the people who worked there were left floundering. If they owned a home, stagnant wages and rising housing prices meant they were likely to have been struggling to meet their mortgage payments even before the layoff. Then the financial crisis hit, and the value of their homes, likely their most expensive assets, plummeted. The young could move away, but for people in midlife the situation was much more difficult; they were trapped in fading communities with few job prospects and recently emptied retirement accounts.
In Russia, the sharp uptick in the mortality rate was attributed in part to an increase in deaths related to alcohol consumption and stress resulting from pessimism about the future. Russian society was in turmoil at the time, in the lead-up to and aftermath of the dissolution of the Soviet Union in 1991. Protests sprang up across the Soviet Union, and by 1999 real GDP had fallen by 40%. People in the society saw their country’s prominence in the international community take a very abrupt hit, and there was massive uncertainty about the future.
Now we’re seeing a similar loss of hope among white Americans. In 2010, the Pew Research Center found that 57% of whites believed their economic situation would improve in the coming year, while 81% of blacks did. The African American community was in many ways hit harder by the financial crisis than whites were, but their 45-54 death rate decreased by 2.6% per year. Europe was hit hard, but mortality rates in its developed countries continued to fall by 2% each year. White Americans were experiencing something that few other groups seemed to express: a loss of hope.
The exceptional pessimism of white Americans was likely related to a sense of historical decline. Fifty years ago a white person could have a pretty good life with just a high school education. If they worked hard and saved right, they could buy a home and send their kids to college. But the costs of housing, healthcare, and college rose, and real wages did not rise with them. That means that most white adults had to work harder than their parents worked to get the same things, and achieving more became steadily more difficult. This is the main thing that separates the experience of white America from that of the rest of the country — they know what meritocratic bliss feels like, and only now face a world in which opportunity is not the rule. Some of these people have lost their middle class status, but what most of them lost is the sense that they and their children can join the middle class, and that is far more devastating.
How one epidemic caused another
Americans have been reporting higher and higher levels of neck pain, back pain, chronic joint pain, and sciatica for decades. This is partly related to the well-documented rise in obesity in America, but other health factors are thought to play a role as well. Some patients exaggerate the pain they experience, but physicians estimate that these represent only about 15-20% of cases. The pain may also be a response to people’s financial distress, though it is not understood whether this relationship is psychosomatic or not.
Partly in response to the professed rise in pain, many physicians started calling for changes in pain management. After all, pain is a risk factor for depression and suicide: its implications for other areas of health are enormous. Hospitals and private practices began to pay closer attention to how much pain patients reported, to treat pain as a fifth vital sign, and even incentivize physicians to keep their patients pain free.
At the same time, patterns were brewing in the pharmaceutical industry that did not bode well for American health. A man named Arthur Sackler began advertising to doctors at a far more sophisticated level than had ever been practiced before. In 1996, his family’s company, Purdue Pharma, released a controlled-release oxycodone tablet called OxyContin. Thanks to the advertising techniques Sackler pioneered — including telling patients to “ask their doctor” for this or that drug — OxyContin was proclaimed loudly to be the answer to the epidemic of pain.
What was not understood at the time was the immense potential of OxyContin patients to develop an addiction to the drug. This was not an accident: Purdue had lied about the addictive properties of OxyContin. In 2007 the company was brought up on charges of misleading the public, and three of its executives pled guilty. In one of the largest pharma settlements of all time, the company was forced to pay $600 million in damages. Despite the settlement, the Sackler family, which still owns Purdue, is currently 16th on Forbes’ list of the richest American families.
Prescriptions for opioid painkillers rose and rose, but many Americans didn’t use their entire prescriptions. They would take the pills for a few days and then stop, and the mostly-full bottles began to accumulate in medicine cabinets across America. This created a good environment for abuse. More than half of opioid abusers obtain the medication from someone with a prescription, which means that the pills doctors thought were going to stem the pain epidemic were actually helping to fuel addiction.
The problem became extremely serious very quickly, with 18,893 Americans dying from overdoses of prescription opioid medication in 2014. And while opioids are now the leading cause of accidental drug overdose deaths, they have also fuelled the flames of another drug epidemic: heroin. Four in five new heroin users started with prescription opioid painkillers, and 10,574 people died from heroin overdoses in 2014. Drug cartels like the Xalisco brothers saw an opening in communities with high prescription rates for opioid painkillers, and started flooding them with cheap black tar and white powder heroin to fill a demand that had not existed before.
Overdose deaths rose with opioid prescriptions in communities across the country, but there are gaps in our healthcare system that make some areas even more vulnerable. Studies show that long-term use of addiction maintenance drugs like buprenorphine or methadone is the most effective method for treating opioid addiction, even more effective than rehab. If you live in a rural area, however, it is likely that you will be unable to reap the benefits of these miracle maintenance drugs: 90% of physicians’ offices with waivers to prescribe buprenorphine are in urban counties. While buprenorphine is incredibly effective, the overdose-treatment drug naloxone is even more incredible: it completely counteracts the effects of an opioid overdose with no side effects except immediate-onset withdrawal. Unfortunately, it too has been difficult to come by in rural areas, providing another gap in the healthcare system for addicts to fall through.
The rural rate of suicide is nearly double that of urban areas. Many factors contribute to this statistic: one is that mental health problems tend to be more stigmatized in rural areas. The threat of being treated differently after revealing their condition prevents many with mental health issues from seeking treatment. And even if people in rural areas want to seek treatment for mental health issues, they may not have access; 60% of rural Americans live in areas with a shortage of mental health professionals. They are also ill-served by the importance of individual autonomy in rural communities, which makes those with depression less likely to think of themselves as needing to ask for help. Finally, access to guns is much higher in rural areas, and it has been repeatedly proven to be associated with higher rates of suicide.
The role of privilege
The fact that the group most affected by this spike in the white mortality rate had high school education or less suggests that they were low on the income spectrum, members of a group whose privileges are few. The one privilege they did have was their skin tone, and even that seems to have worked against them here.
Since the healthcare system was developed in this country, white people have had privileged access to it. Robert Morrison, the chief of National Association of State Alcohol and Drug Abuse Directors (NASADAD), said “the [healthcare] system is built for white males.” In 2005, the percentage of African Americans without health insurance was almost double what it was for white non-Hispanics. Doctors and nurses also tend not to practice in communities of color, leaving them underserved. The lack of adequate healthcare services means that the absolute mortality rates are much higher for African Americans and Latinos and every other racial minority.
But the differences do not stop with access to medical care. Even once they’re in an appointment with a physician, white people are treated differently. And this is where mortality found its back door into the white community. White people are significantly more likely to be prescribed opioid pain medication than any other racial group, nearly 50% more likely than blacks or Hispanics.
This disparity may mean that African Americans have suffered more from their illnesses for decades, but it also provided them with a modicum of protection from the opioid epidemic. Addiction is a serious problem in most minority communities, but the rise in heroin and opioid use in the past 20 years has actually been driven by whites, and the overall mortality rates of all other racial groups has continued to drop. Whites die at almost twice the rate of African Americans from drug overdose, and three times the rate of Hispanics.
Similarly, the suicide rate for black men fell between the years 1999-2013 but for white men it rose by 28%. For white women, the rise was 60%. This is alarming because suicide was already disproportionately a white problem. Whites had more than twice the suicide rate of most other racial groups at the beginning of this period, and almost three times by the end. The only group close is Native Americans, whose communities face many of the same challenges as rural white communities as they struggle to integrate into an economy and a society in the midst of a major transformation.
This difference cannot be explained by a genetic link. White people have the lowest rate of depression, just over half that of African Americans. It is only in the behavior of committing suicide that whites stand out, and while they have some influence, genetic factors alone cannot determine behavior. Additionally, there seems to be no evidence of a cultural explanation: African Americans and whites do not differ in their perceived stigma towards mental health or towards mental health treatment.
Some say that the disparity in suicide too is the result of privilege. Many white people grow up never facing the same challenges and adversities as their peers in less advantaged groups, and this may make them less equipped to deal with hardship when it comes their way. Living requires living through pain, whether it be chronic back pain, job loss, or mental illness. It also requires living with shame — and learning to overcome it. Some research shows that older gay men may be more likely to seek treatment for stigmatized conditions. The authors of the study suggested that their experience with one type of stigma prepared them to better deal with other types when confronted with them. White men, the least stigmatized group of all, lack any such preparation, and that seems to be the only compelling explanation for why in 2014 they accounted for seven in ten completed suicides.
More than any other community, the white community has always expected its future to be bright. Based in their experience of times being good, they believed that they always would be. But for the past 20 years, they haven’t been for many. White expectations may be their biggest vulnerability to the diseases of despair that bring the epidemic of grief. The fact that blacks have a much lower standard of living, a much higher rate of depression, and a much lower suicide rate implies that suicide has everything to do with a victim’s expectations, where he or she expects to go relative to where they have been before.
Another Part of Life?
There have been some victories in the fight against this rise in mortality among American whites. In July 2016, Congress passed the Comprehensive Addiction and Recovery Act, which expands the availability of naloxone and helps to improve drug monitoring programs that reduce the distribution of excess pain medication. Attitudes around mental health and addiction have also progressed as more families choose to break the stigma and name the real causes of their loved ones’ deaths in often deeply moving obituaries. Overall, though, the changes have been shallow and fail to address some of the fundamental causes of addiction and suicide.
Scientists have learned far more about the causes of addiction than many people realize. In his book In the Realm of Hungry Ghosts, Dr. Gabor Maté writes about the importance of childhood development in the formation of addiction. Children who experience too much stress at an early age, especially those who face early disruption of care or childhood trauma, do not properly develop opioid receptors in their brains. The effects last into adulthood, when these patients begin to fixate on the chemical rewards for any behavior from shopping to heroin injection. Many do not choose innocent fixations — among adolescent substance abusers, three in four experienced at least one childhood trauma. Far from being the result of any innate failings, their addictive behavior is the result of their experiences and the environments in which they were brought up.
Addiction has its social roots as well. Bruce Alexander writes about Native American populations, well-known for their high rates of substance abuse. What is less well-known is that addictive behavior was virtually non-existent among them before the arrival of the Europeans. Rather than an economic explanation, he points to a phenomenon he terms dislocation, a feeling of having lost one’s place in the world. Native societies were cohesive and clearly ordered — everyone had his or her defined place, which was always important to the society and always contained the possibility for advancement. When they became restricted to their reservations and denied many of their native practices, this cohesion and sense of purpose was shattered. This situation is increasingly reminiscent of the position of rural white people in modern society, stranded in shrinking territories far from their traditional sense of purpose.
The effects of trauma and dislocation do not halt with addiction — both are risk factors for suicide as well. The fact that the only group with a suicide rate comparable to that of whites is the Native Americans is evidence that their positions bear some similarities and that they face many of the same risks. Hopelessness about the future and the sense of experiencing a decline in prominence cause both phenomena to manifest. And trauma during development, while not a white issue, feeds both afflictions.
We know that pain is a risk factor for both suicide and opioid addiction, and that depression is a risk factor for opioid abuse — the phenomena of addiction and suicide are deeply related, their causes often indistinguishable.
Often we think of death as just another part of life, but history has shown us that victories can be won in the war against it through policy changes. Mortality among low-income people is lowest in counties with high government spending, suggesting that social programs help to avoid deaths in this demographic. We can stem the tide of rising mortality by providing paid family leave to reduce the strain on mothers and infants at the time of birth. We can provide services to victims of trauma. We can invest in new jobs and a new sense of purpose for those left behind by the financial crisis. We can extend mental health and addiction treatment to the communities that lack them and eliminate the surrounding stigma. And all of these policies would help the disadvantaged of every shade — not just rural whites.
Cover photo courtesy of Flickr/Andreas Mortonus
